Worldwide, 15% of couples experience infertility, with around half of these attributable to the male. Male infertility is complex, and studies have consistently shown that the condition is influenced by a range of biological and environmental factors. A new study published in Diagnostics in March 2025 analyzes the role of infections, inflammation, and autoimmune mechanisms in male fertility, promoting their understanding and emphasizing the importance of improving diagnostic methods.
Fertility and the immune system
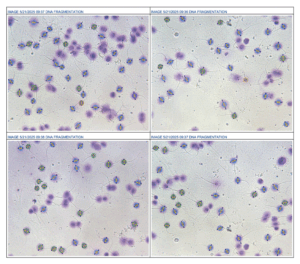
As noted by the study authors, while immunological factors affect reproduction, they are still poorly understood. The immune system in the testes plays an important role in protecting developing sperm, as they are isolated within the blood-testis barrier, a structure that also provides an immunosuppressed environment. However, changes in this environment, due to factors such as infections or inflammation, can impair sperm function and fertility. Infections like prostatitis, urethritis, and epididymitis, often caused by sexually transmitted bacteria or uropathogens, contribute to these issues. Autoimmune diseases and immunosuppressive treatments have also been shown to affect male fertility, though the evidence is scattered, and further research is needed to understand the mechanisms involved.
For this study, a narrative review of literature from the past 10 years was carried out, including studies focusing on testicular and epididymal disorders, immunological impacts, and therapeutic approaches. The study continues to reinforce that conditions such as epididymitis, vasectomy, testicular injury, and previous surgeries can provoke inflammatory reactions, leading to the formation of antisperm antibodies (ASA) and increased oxidative stress. More specifically, sperm immobilizing antibodies prevent sperm from moving effectively within the female reproductive tract. Infections, particularly those caused by sexually transmitted bacteria or urinary pathogens, often result in epididymo-orchitis, a significant factor in male infertility.
Bypassing ASA
As the authors note, while standardized methods for ASA testing are still lacking, intracytoplasmic sperm injection (ICSI), and intrauterine insemination (IUI) can be promising in addressing immune-related infertility. Since IUI bypasses cervical mucus, it has been found to improve sperm movement in ASA-positive cases with significantly higher live birth rates when compared to natural conception. When ICSI is used, ASA does not impact fertilization, embryo development, or live births, and both ASA-positive and ASA-negative men experience similar success rates. However, men with ASA had lower IVF success rates when compared to men without. This suggests that ICSI might be a better option for ASA-positive patients, although further studies are needed to confirm this.
The study’s key takeaway
This study contributes to our understanding of infections, inflammation, and autoimmune factors in male infertility and recommends treatment paths that can help ASA-positive men achieve parenthood. While assisted reproductive technologies offer promising solutions, there is still much that’s unknown about the underlying mechanisms of infertility. The study highlights the importance of improving diagnostic methods and understanding immune-pathological mechanisms to improve fertility outcomes – and its social implications.
Stay updated with the latest in fertility research and technology. Explore the latest sperm testing solutions available for fertility clinics, sperm banks, and laboratories here