An excellent series of “Questions and Answers” that came through our Austrian Distributor regarding cutoffs and reference ranges:
Question:
We are presenting the SQA-V at a conference and I fear that the “reference” range cutoff values for morphology will be questioned. The technical bulletin you sent says there is high correlation between SQA and humans…..however, human semen analysis is prone to massive CV’s and errors. It is hard to believe (and certainly from our data as regards motility and morphology) there is any correlation between a human and a machine value, as machines are far more accurate.
Answer:
WHO established reference ranges based on the results of studies conducted on a population of fertile men. What was done is that the lowest 5% of the values (5th centile) from this group was used as the lower reference limit (please see below). This is a purely clinical study involving the semen assessment of men with PROVEN FERTILITY which is quite different from the scope of the SQA-V technology. The SQA-V technology provides automated semen analysis comparable to the manual standards, based on the WHO guidelines for semen analysis. The SQA-V technology is therefore presented as comparable to the current laboratory standard (manual) with decided advantages such as: Automation, speed, ease of use, standardization, objectivity, precision, and accuracy that is not depend on the proficiency level of the operator. Because the only current globally recognized standard is manual semen analysis based on WHO guidelines, this was used as the gold standard in the SQA-V algorithm development trials. Without a standard with which to develop an automated system, the results will be far from reality and will not stand up to validation or comparison studies. Hence, in the course of algorithm development, MES strictly followed the WHO recommendations for manual semen analysis. As a result, the manual results used for establishing the SQA-V algorithms are (and have proven to be) more accurate than would be expected from any given laboratory. Fact is, this algorithm development is not a simple correlation, but a much more complex and interrelated process.
Reference ranges and reference limits. Data characterizing the semen quality of fertile men, whose partners had a time to pregnancy of 12 months or less, provided the reference ranges for this manual. Raw data from between about 400 and 1900 semen samples, from recent fathers in eight countries on three continents, were used to generate the reference ranges. Conventional statistical tradition is to take the 2.5th centile from a two-sided reference interval as the threshold below which values may be considered to come from a different population. However, a one-sided reference interval was considered to be more appropriate for semen, since high values of any parameter are unlikely to be detrimental to fertility. The 5th centile is given as the lower reference limit, and the complete distribution for each semen parameter is also given in Appendix 1. (WHO 5th ed., p. 3).
Comment 7: There may be regional differences in semen quality, or differences between laboratories; laboratories should consider preparing their own reference ranges, using the techniques described in this manual. (WHO 5th ed., p. 224).
Question:
If the results with consistent human counting errors were used to determine the lowest 5th-centile WHO 5th morphology value of 4% and if the SQA-V doesn’t have massive errors, what is the lowest 5th-centile range from the SQA analyzed samples? It would have to be different from the manual analyses. So if the accuracy is improved using a SQA, then the precision may be lifted (or lowered) to form a level that over a large number of samples becomes the new reference level.
Answer:
Just to reiterate a point, the WHO reference limits were established based on the test results from a population of HEALTY MEN with proven fertility. In contrast, the population of our clinical trials consists of men who applied for medical assistance due to infertility problems. Some of them are healthy as the fertility problem is the result of the female, others are infertile. So 5th centile in this population is different when compared to the healthy group WHO used to establish reference limits.
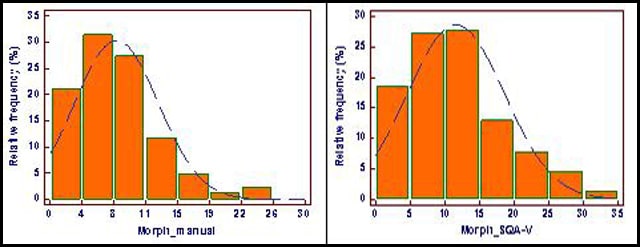
Please find below two distribution graphs: One shows manual and the other SQA-V Morphology assessed in a recent trial conducted in France (Nantes trial data) on 250 patients. You will noted that the distribution patterns of the manual and automated results are quite similar. Also, you will note that approximately 21% of the samples assessed manually fall below the 4% cutoff (WHO 5th) and 18% of the samples assessed automatically fall below 5% cutoff. Based on this extrapolation, 20th centile instead of 5th centile can be used in this group, and the morphology cutoff for the SQA-V can possibly be shifted from 4% to 5% if the lab will find it reasonable.
Question:
It’s impossible to believe that if there are minimal sampling errors, the human derived cut off of 4% (lowest 5% of all values analysed) is the same. Same will have to be determined for the lowest 5% of all measured values for sperm count and sperm motility, and see where the numerical cut off is for these lowest 5th-centile ranges.
Answer:
This question relates to the difference between accuracy and precision. Even if the precision of the manual method is low, averaging multiple results will bring a result close to the “true” value (accuracy). To establish a reference value, multiple results are used, so it is quite accurate even though precision may not be high. Where precision becomes very important is in routine practice where EVERY individual result needs to be reproducible. Concerning the 5th centile, I would like to emphasize that it is not applicable to patients with potential infertility problems. I think it is well demonstrated in the graphs above.
The questions at the end of your e-mail are addressed by the explanations above I believe. Please let us know if this answers your questions.
Best regards,
Dr. Lev Rabinovitch ~ Chief Technology Officer