Abstract Presented at the 2011 AACC Meeting in Atlanta, GA. DOWNLOAD STUDY HERE
Semen analysis is one of the clinical laboratory tests which has significantly benefited from automation. Manual counting methods, motility and morphology testing often resulted in prolonged turn-around-times and left our Laboratory faced with challenges of maintaining consistency in result reporting among Technologists. The projected shortage of laboratorians also weighed in our decision to automate, since finding skilled help might be a problem in the future. We decided to automate semen analysis testing with Medical Electronics SQA-V Semen Analyzer. This decision was the result of our laboratory’s use of LEAN practices which identified what we needed in order to streamline testing while providing clinicians with accurate and consistent results. Our main goals at this time were decreasing turn- around times and cost savings.
The SQA-V Semen Analyzer is a bench top device that determines the total sperm count, motility and morphology of a specimen in less than 2 minutes. The SQA-V technology is based on the principle of electro-optical signal processing in conjunction with algorithms built into the software. A disposable testing capillary is filled with a liquefied, well mixed sample inserted into the analyzer for testing. We are currently running fresh specimens on the analyzer. QwikCheck beads at two known concentrations are run as the quality control material.
37 patient samples were used to validate the automated system. This included a representation of both normal and abnormal specimens. The manual testing was performed by all members of the staff trained in manual semen analysis using WHO 3rd classification. Training the staff on the automated system was completed in 5 days and after implementation we were immediately able to meet our new turn-around-time goal consistently. Previously, with manual semen analysis, the average TAT was 3 days due to delays involved in manual processing, such as transport for staining and microscopic examination. Automating the process has decreased the turn-around-time for the majority of our specimens to under 3 hours. (See Figure 1).
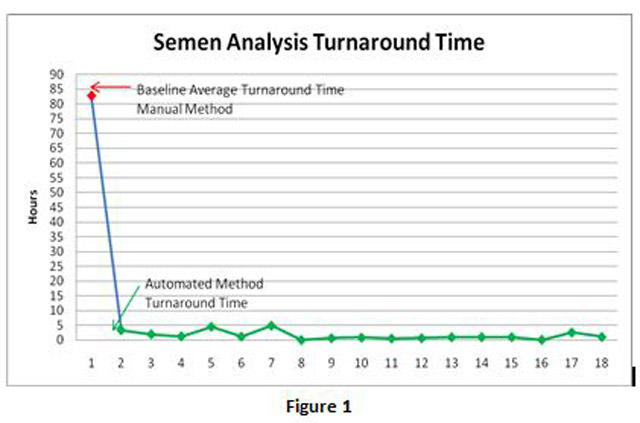
Through automation, we were able to reduce our average turn-around-time per case from 82 hours to 3 hours. Annualized, this freed up 0.5 FTE. We performed 161 cases in 2010. Overall, labor costs for semen analysis were reduced by $14,560.00.
Automating semen analysis has enabled our Laboratory to offer testing on demand while eliminating many of the delays involved in manual processing. It has enabled us to maximize our resources, so that now our laboratorians are no longer spending hours working on a single specimen and are free to perform other tasks. Our physicians can now rely on having accurate test results consistently available in less than 3 hours. Our staff oriented quickly, with minimal training and automating the process has proven to be a major boost to staff morale. Maintaining competency will continue to remain a challenge since we will still need to perform manual testing on short samples. But most importantly, process improvement through automation brings us one step closer to achieving our vision; to be a premier laboratory, implementing advances in laboratory medicine, while providing exceptional service to exceed the needs and expectations of the people we serve.