A semen analysis is the cornerstone of male fertility evaluation. It measures several key parameters that provide a complete picture of sperm health. Understanding what each metric means can help patients and providers make informed decisions about next steps in family planning.
- Sperm Concentration
Also known as sperm count, this measures the number of sperm in each milliliter of semen. Low concentration (oligozoospermia) can make conception more difficult, while normal or high counts increase the odds—though quality matters just as much as quantity.
- Motility
Motility measures the percentage of sperm that are moving. Poor motility (asthenozoospermia) can limit a sperm’s ability to reach and fertilize the egg.
- Progressive Motility
Not all movement is effective—progressive motility measures the percentage of sperm swimming forward in a purposeful path. This is crucial for natural conception.
- Morphology
Morphology assesses the shape and structure of sperm. Abnormal shapes may reduce fertilization potential. The WHO 6th Edition guidelines set clear reference ranges for what’s considered “normal” morphology.
- Motile Sperm Concentration (MSC)
MSC combines count and motility, showing how many sperm in a sample are both present and moving. It’s a strong indicator of overall fertilizing potential.
- Progressive Motile Sperm Concentration (PMSC)
PMSC refines this further—measuring how many sperm are both moving forward and present in sufficient numbers. This is one of the most predictive metrics in male fertility.
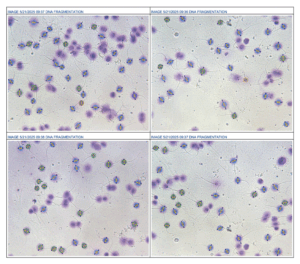
- DNA Fragmentation Index (DFI)
An advanced metric that measures breaks in sperm DNA. High fragmentation can affect embryo development and pregnancy outcomes, even if other parameters look normal.
Why These Numbers Matter
No single parameter tells the full story. Fertility specialists look at all results together, often repeating tests to confirm accuracy. The insights gained guide treatment—from lifestyle changes to assisted reproductive technologies.
With modern technology, such as FDA-cleared automated semen analyzers and at-home sperm tests, these parameters can be measured accurately and conveniently—bringing clarity to couples earlier in their fertility journey.